What we treat
We’re specialists in neuromusculoskeletal physiotherapy, which covers:
Achilles Tendonitis / Tendinosis
1. DEFINITION & ANATOMY
The Achilles tendon is the strong, fibrous cord that connects the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus). It plays a crucial role in walking, running, and jumping by helping to push off the ground. Pain in this area is commonly grouped under the term Achilles tendinopathy, which describes pain localised at the back of the heel or slightly above it. This condition typically presents as either Achilles tendonitis, an acute inflammatory irritation often reacting to a sudden increase in load, or Achilles tendinosis, a more degenerative condition related to chronic overload that causes changes in the tendon’s structure. Tendinopathy can affect the middle portion of the tendon (mid-portion) or where it attaches to the heel bone (insertional).
2. SYMPTOMS & SIGNS
- Pain located at the back of the heel or a few centimetres above it.
- Morning stiffness or significant “first-step” pain upon getting out of bed.
- Tenderness when touching the area, with possible warmth, swelling, or a noticeable thickening of the tendon.
- Pain that increases with activities that require push-off, such as hopping, running, or walking uphill.
- A crackling or grating sensation (crepitus) may be present in acute cases.
- Reduced power or a feeling of weakness in the calf muscle.
- Stiffness that eases with gentle movement but worsens after a period of heavy or sustained activity.
- For insertional tendinopathy, pain can be aggravated by shoes rubbing against the back of the heel.
3. CAUSES & RISK FACTORS
- Sudden increases in training intensity, such as adding volume, speed, or hill work too quickly.
- Repetitive overload from activities like running and jumping without adequate recovery.
- Poor strength in the calf muscles or supporting muscles around the hips.
- Limited ankle flexibility, particularly the ability to bend the foot upwards (dorsiflexion), and tight calf muscles.
- Altered foot mechanics, such as flat feet or overpronation (foot rolling inwards excessively).
- Returning to sport or activity too quickly after a layoff period.
- Certain medications (e.g., fluoroquinolone/quinolone antibiotics, statins) can increase risk.
- Higher incidence in males aged between 30 and 60.
- Regularly training on hard surfaces or using unsupportive footwear.
- Other factors like a high BMI or systemic conditions such as diabetes or inflammatory arthritis.
4. HOW PHYSIOTHERAPY HELPS
- Thorough Assessment: We evaluate your walking and running pattern (gait), foot posture, ankle mobility, and calf strength and endurance. This helps us make a precise diagnosis and rule out other issues like plantaris involvement, bursitis, or a partial tear.
- Load Management Plan: We will help you temporarily modify aggravating activities like speed work, hills, or jumping, while showing you how to maintain your general fitness safely.
- Progressive Tendon Loading: Your treatment will be built around an evidence-based exercise programme. This includes specific calf strengthening exercises (like eccentrics and heavy slow resistance), isometrics for pain relief, and a gradual progression to jumping and running drills.
- Manual Therapy: We may use hands-on techniques such as soft tissue massage and joint mobilisations to improve mobility and reduce symptoms where appropriate.
- Adjuncts: We can provide taping for support, advise on short-term heel lifts (especially for insertional cases), and may use shockwave therapy if your condition is not progressing as expected. We also offer guidance on footwear and orthoses.
- Education: A key part of recovery is understanding your condition. We will teach you how to pace your activities, warm up correctly, and monitor your symptoms using acceptable pain guidelines.
5. TIMELINE / EXPECTED RECOVERY
- Reactive/Acute Tendonitis: With early and effective load management and targeted exercises, symptoms often improve significantly within 4–6 weeks.
- Tendinosis/Chronic Tendinopathy: This condition requires a more patient approach. It typically takes 8–12 weeks or more of a consistent, progressive loading programme to see meaningful improvement, with full resolution sometimes taking several months.
- Insertional Cases: Tendinopathy at the heel bone attachment can sometimes progress more slowly than mid-portion issues.
- Your outcome is strongly predicted by how consistently you perform your exercises and manage your activity levels.
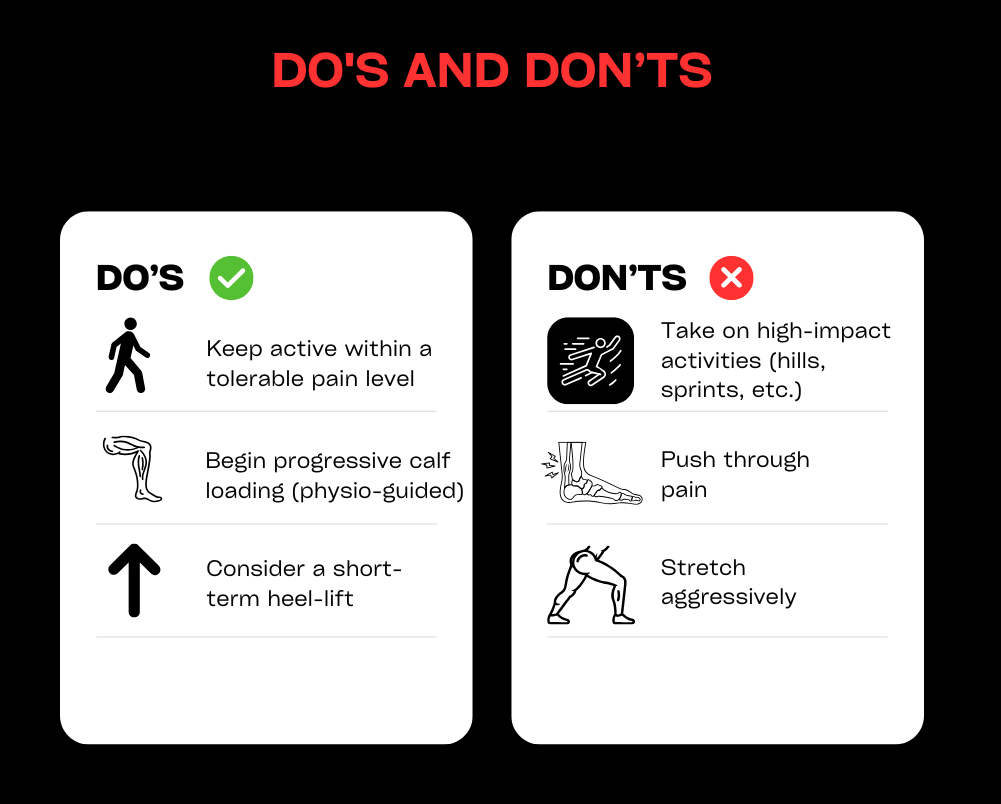
6. SELF-HELP & PREVENTION
- Temporarily reduce activities that cause significant pain, but keep moving within comfortable limits (e.g., cycling, swimming, or walking on flat ground).
- Begin gentle calf-loading exercises as advised by your physiotherapist, starting with isometrics and moving to slow, controlled calf raises.
- If your calves are tight, perform regular gastrocnemius and soleus stretches. Initially, avoid stretching that causes direct compression pain for insertional cases.
- Use temporary heel lifts or wear shoes with a slightly higher heel to reduce strain on the tendon in the early stages.
- When reintroducing activities like running, do so gradually. Be cautious with sudden increases in hills, speed work, or jumping.
- Work on strengthening your hip and foot muscles, check your footwear for signs of wear, and consider orthoses if overpronation is a factor.
- Use ice or heat for short periods for symptom relief, and prioritise your overall training load management and sleep for better recovery.
7. WHEN TO SEE A PHYSIO OR SPECIALIST
- If pain continues for more than 2–4 weeks despite self-care, or if it keeps returning when you increase activity.
- If you experience marked swelling, hear or feel a sudden “pop,” or have significant difficulty pushing off your foot (this could indicate a tear and requires urgent assessment).
- If you have pain at night, or if redness and warmth do not settle, which may suggest an infection or an underlying inflammatory condition.
- If the pain is significantly impacting your sport, work, or daily life, or if you are uncertain about the diagnosis.
- Consider a specialist review if your symptoms fail to improve after a well-supervised 12-week loading programme with a physiotherapist.
Ankle sprains
1. DEFINITION & ANATOMY
An ankle sprain occurs when the strong ligaments supporting the ankle joint are stretched beyond their limits and torn. The most common type is a lateral sprain, caused by the foot turning inwards (inversion), which affects ligaments on the outside of the ankle like the ATFL and CFL. Less common are medial sprains (from the foot turning outwards) or high ankle (syndesmotic) sprains, which involve ligaments above the ankle joint. Ligaments provide stability and proprioception (your sense of joint position). Sprains typically happen from twisting on uneven ground or landing awkwardly during sport, often resulting in swelling and bruising around the ankle bones (malleoli). Without proper rehabilitation, sprains can lead to lasting deficits in mobility, strength, and balance, significantly increasing the risk of it happening again.
2. SYMPTOMS & SIGNS
- Pain on the outer or inner side of the ankle, depending on which ligaments are injured.
- Visible swelling and bruising, which may track down into the foot and toes.
- Tenderness to touch over the affected ligaments.
- Difficulty or inability to put weight on the foot.
- Reduced range of motion, especially when trying to pull your foot upwards towards your shin (dorsiflexion).
- A feeling of instability, unsteadiness, or the ankle “giving way.”
- Stiffness in the morning or after periods of rest.
- Pain with dynamic movements like hopping, cutting, or changing direction.
- A high ankle sprain may cause pain above the ankle joint, which is worsened by twisting the foot outwards.
3. CAUSES & RISK FACTORS
- Twisting or rolling the ankle during sport (inversion or eversion injuries).
- Walking or running on uneven surfaces.
- A history of previous ankle sprains.
- Poor balance or proprioception (joint position sense).
- Inadequate warm-up before activity.
- Weakness in the supporting muscles, particularly the peroneal and calf muscles.
- Limited ankle mobility or flexibility.
- Wearing inappropriate or unsupportive footwear.
- Participation in high-risk sports like football, netball, basketball, and trail running.
- General fatigue, which can lead to poor movement control.
4. HOW PHYSIOTHERAPY HELPS
- Assessment: We will perform a thorough evaluation to grade the sprain (from mild Grade I to a complete tear Grade III), screen for a possible fracture using the Ottawa Ankle Rules, and differentiate between lateral, medial, or high ankle injuries.
- Acute Care Plan: We provide guidance based on modern principles (PEACE & LOVE), advising on protected weight-bearing, the appropriate use of compression and elevation, and when to use a brace, taping, or crutches.
- Restore Mobility: Treatment includes early, pain-free range of motion exercises (like drawing the alphabet with your foot) and hands-on manual therapy or joint mobilisations to restore normal movement.
- Strength and Control: We design a progressive loading programme to strengthen key muscles (peroneals, calf, tibialis posterior) and guide you through a safe return-to-run and change-of-direction plan.
- Balance & Proprioception: A crucial part of your recovery will be targeted neuromuscular training, using exercises like single-leg balancing and wobble boards to retrain your joint control and significantly reduce re-sprain risk.
- Education and Adjuncts: We help manage swelling, provide soft-tissue techniques, and educate you on load management, correct footwear or bracing, and the clear milestones you need to hit before progressing your activity.
5. TIMELINE / EXPECTED RECOVERY
- Grade I (Mild): Most symptoms typically settle within 1–3 weeks, with a return to sport often possible in 2–4 weeks with consistent rehabilitation.
- Grade II (Moderate): Recovery usually takes 3–6 weeks, with a return to sport taking 4–8 weeks or longer, depending on the physical demands of the activity.
- Grade III (Severe) / High Ankle Sprains: These injuries require more time, often taking 8–12 weeks or more. Some may require a period of immobilisation or specialist input.
- Engaging in early, structured rehabilitation is the most effective way to prevent chronic instability and reduce the high risk of re-injury.
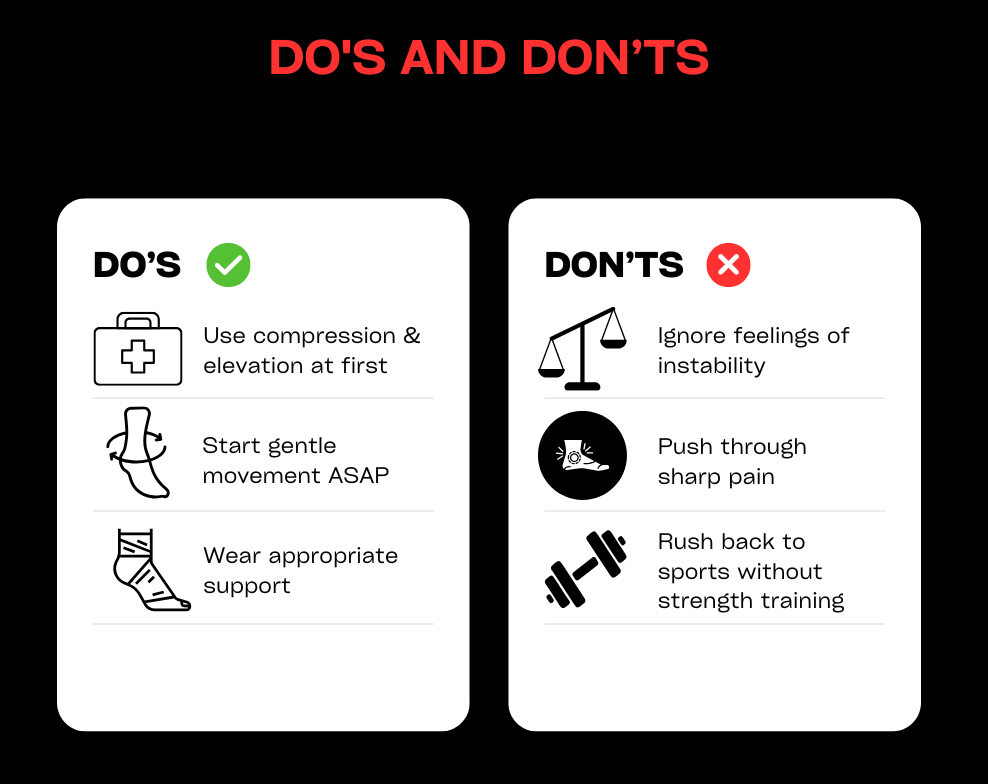
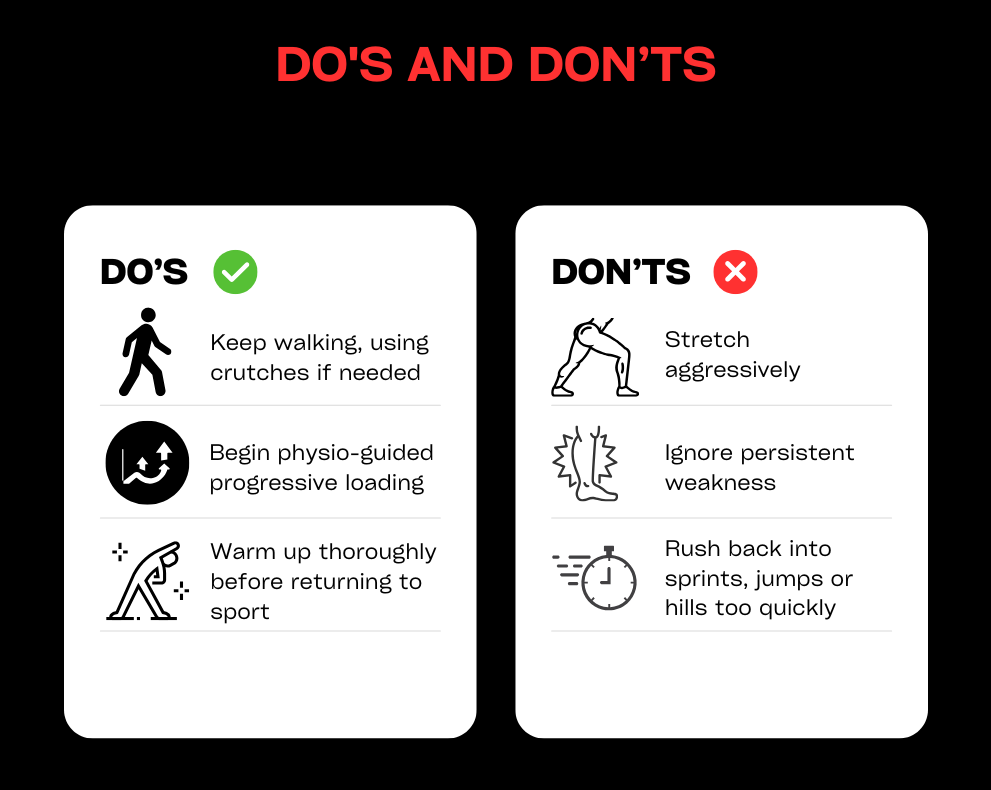
6. SELF-HELP & PREVENTION
- In the first 48–72 hours, follow the principles of protection, relative rest, compression, and elevation. Avoid things that can increase swelling, like heat, alcohol, and deep massage.
- As soon as you can without pain, begin gentle range-of-motion exercises like ankle pumps or drawing the alphabet with your foot.
- Use a supportive lace-up brace or taping when returning to higher-risk activities to provide extra stability.
- As pain subsides, progress to balance exercises and strengthening for your calf and peroneal muscles.
- Reintroduce running, cutting, and jumping gradually, ensuring you meet strength and stability milestones before increasing intensity.
- Choose supportive footwear for your sport and daily activities.
- Maintain good strength in the muscles around your hips and knees to improve overall lower limb control.
7. WHEN TO SEE A PHYSIO OR SPECIALIST
- If you are unable to put any weight on your foot immediately after the injury or the next day, as this may indicate a fracture.
- If you experience severe swelling, a visible deformity, or the pain, swelling, or instability does not improve after 1–2 weeks.
- If you have specific tenderness above the main ankle joint (syndesmosis) or significant pain on the inner side of your ankle.
- If your ankle frequently “gives way,” locks, or catches during movement.
- If your recovery stalls or you are not progressing after 4–6 weeks of a self-managed rehab programme, or if you need expert guidance for returning to sport safely.
Calf strains / tears
1. DEFINITION & ANATOMY
A calf strain or tear is an injury to the muscle fibres at the back of the lower leg. The calf is made up of two main muscles: the gastrocnemius and the soleus. The gastrocnemius is the larger, more superficial muscle that crosses both the knee and ankle joints; it is most active with the knee straight during explosive push-offs. The soleus is a deeper, smaller muscle that works hardest when the knee is bent, playing a key role in endurance and standing posture. Strains often happen during sudden movements like sprinting, pushing off for a tennis shot, or running uphill. Accurately identifying which muscle is injured is crucial as it guides the specific exercises needed for an effective recovery.
2. SYMPTOMS & SIGNS
- A sudden, sharp pain in the back of the lower leg, sometimes accompanied by a pulling or tearing sensation.
- Difficulty walking normally or pushing off the foot.
- Localised tenderness when pressing on the muscle belly.
- Swelling and/or bruising, which may develop over 24-48 hours.
- Stiffness and pain after periods of rest.
- Pain when performing a calf raise (standing on your tiptoes).
- Reduced power or a feeling of weakness in the calf.
- A “pop” sensation may be felt at the moment of injury.
- Gastrocnemius pain is often worse with the knee straight, while soleus pain can be more noticeable with the knee bent.
- In severe cases, a visible gap or defect may be present in the muscle, and you may have a significant limp.
3. CAUSES & RISK FACTORS
- An inadequate warm-up before exercise or sport.
- Sudden increases in running speed, distance, or intensity.
- Explosive changes of direction required in sports like football or squash.
- Underlying tightness in the calf muscles or limited ankle mobility.
- Fatigue, which can lead to poor muscle control and overload.
- A history of a previous calf strain.
- Poor strength or endurance in the calf muscles.
- Weakness in supporting muscles, such as the glutes and hamstrings.
- Poor running mechanics or wearing unsuitable footwear.
- A sudden introduction of uphill running.
- Dehydration or not allowing enough recovery time between hard sessions.
4. HOW PHYSIOTHERAPY HELPS
- Assessment: We will perform a detailed examination to grade the strain (I-III), differentiate between a gastrocnemius and soleus injury, and screen for more serious issues like a complete tear or red flags for a DVT (Deep Vein Thrombosis).
- Acute Management: We guide you on a plan of relative rest, compression, and elevation. We may recommend crutches or temporary heel lifts to reduce load and manage pain, prioritising pain-modulated loading over complete rest.
- Restore Mobility: Your treatment will include gentle, pain-free range of motion exercises, soft-tissue work, and joint mobilisations where needed to restore flexibility without stressing the healing tissue.
- Strength & Loading: We will create a phased exercise programme starting with gentle isometrics, progressing to controlled calf raises (both with the knee straight for gastrocnemius and bent for soleus), and building up to heavy slow resistance, jumping, and running drills.
- Return-to-Sport Criteria: Before you return to your sport, we will ensure you meet key criteria, including symmetrical strength and endurance, and the ability to tolerate hop tests, sprints, and changes of direction.
- Education: We empower you with knowledge on how to pace your recovery, perform effective warm-ups, manage your training load, and monitor symptoms to prevent re-injury.
5. TIMELINE / EXPECTED RECOVERY
- Grade I (Mild): Recovery for everyday activities is often within 1–2 weeks. A return to sport with a full rehabilitation programme typically takes 2–4 weeks.
- Grade II (Moderate): These injuries usually require 3–6 weeks or more, depending on the demands of your activities and adherence to the rehab plan.
- Grade III (Significant Tear): A more severe tear can take 6–12 weeks or longer to heal. Some cases may require medical imaging or a specialist review.
- Following an early, structured loading programme significantly reduces the high risk of re-injury that comes with rushing back to activity too soon.
6. SELF-HELP & PREVENTION
- For the first 48–72 hours, focus on protection, relative rest, compression, and elevation. Avoid aggressive stretching if it causes sharp pain.
- Using small heel lifts in both shoes or wearing shoes with a slight heel can temporarily reduce strain on the calf in the early stages.
- Begin gentle, pain-free isometric contractions as advised. Progress to both straight-knee and bent-knee calf raises as symptoms allow.
- Gradually build your running tolerance. Start on flat surfaces and increase your distance before you increase your speed. Delay hill and sprint work until the later stages of your rehab.
- Maintain good strength in your hips and glutes and work on your ankle mobility. Always include dynamic warm-ups before sport.
- Stay well-hydrated and ensure you have adequate recovery time between hard training sessions.
7. WHEN TO SEE A PHYSIO OR SPECIALIST
- If you heard or felt a distinct “pop,” have significant swelling and bruising, or cannot walk without a severe limp.
- If you can see a visible gap or dent in the muscle, or if you are concerned the Achilles tendon may be involved.
- If pain persists beyond 1–2 weeks, you suffer from recurrent calf strains, or you are unsure which muscle is injured.
- Urgent care is needed if you have calf swelling, warmth, and tenderness with no clear injury, or if you experience unexplained shortness of breath, as these can be signs of a DVT.
Groin strains and sacroiliac pain
1. DEFINITION & ANATOMY
This section covers two related but distinct issues affecting the pelvis and inner thigh. A groin strain is an injury to the muscles of the inner thigh, most commonly the adductor muscles (especially the adductor longus) or the hip flexors. Sacroiliac (SIJ) pain refers to irritation or dysfunction of the sacroiliac joints, which are located where the base of your spine (sacrum) meets your pelvis. This pain can be related to the joint itself or the strong supporting ligaments. Both conditions can be triggered by the hormonal changes and increased load during pregnancy and postpartum, or by sporting movements like sprinting, changing direction, and kicking. A proper diagnosis is essential as the management for each differs, though strengthening the core and hip muscles is a common focus for both.
2. SYMPTOMS & SIGNS
- Groin Strain: A sharp pain in the inner thigh during activities like sprinting, cutting, or kicking; tenderness along the adductor muscles; pain when squeezing your legs together or stretching the inner thigh; possible bruising or swelling; stiffness after rest.
- SIJ Pain: One-sided low back or buttock pain that may refer into the groin; pain that worsens with prolonged standing or walking, rolling over in bed, or climbing stairs; tenderness over the back of the pelvis; pain with standing on one leg.
3. CAUSES & RISK FACTORS
- Pregnancy and the postpartum period, due to the hormone relaxin causing ligament laxity and changes in body load.
- Sudden increases in training intensity or an inadequate warm-up.
- Poor strength in the adductor muscles, hip flexors, deep core, or gluteal muscles.
- An imbalance between the inner thigh muscles (adductors) and outer hip muscles (abductors).
- Participation in sports that involve frequent cutting, kicking, or skating, such as football, hockey, and rugby.
- Poor movement control and coordination.
- A history of a previous groin strain or pelvic pain.
4. HOW PHYSIOTHERAPY HELPS
- Assessment: We perform a detailed evaluation to differentiate between an adductor strain, hip flexor issue, or SIJ-driven pain. We also screen for other potential problems like hip joint pathology or a hernia and consider any pregnancy or postpartum factors.
- Load Management: We help you modify aggravating activities and create a graded plan for your return to running, cutting, and kicking.
- Targeted Exercise: Your rehab will focus on what you need. This may include adductor strengthening (like Copenhagen progressions), core and pelvic stability exercises, and gluteal strengthening. We also address any mobility issues in the hips or spine.
- SIJ Strategies: For SIJ pain, we may recommend a temporary pelvic support belt, teach you specific motor control exercises to improve lumbopelvic stability, and use manual therapy or mobilisations where appropriate.
- Education: We provide advice on posture, optimal sleeping positions, and safe lifting techniques (especially important for perinatal clients), along with clear guidelines for monitoring your symptoms.
- Adjuncts: We may use taping or soft-tissue techniques to manage symptoms. For chronic tendon-related groin pain, shockwave therapy may be an option, but it is not a first-line treatment.
5. TIMELINE / EXPECTED RECOVERY
- Mild Groin Strains: With a proper rehab programme, a return to light sport is often possible within 2–4 weeks.
- Moderate Groin Strains: These typically require 4–8 weeks or more, depending on the demands of your sport.
- SIJ Pain: Symptoms often improve significantly within 4–6 weeks with targeted exercise and load management. Perinatal cases can fluctuate but respond well to tailored support and strengthening.
- Chronic or recurrent cases may require a longer, more progressive programme lasting 8–12 weeks or more.
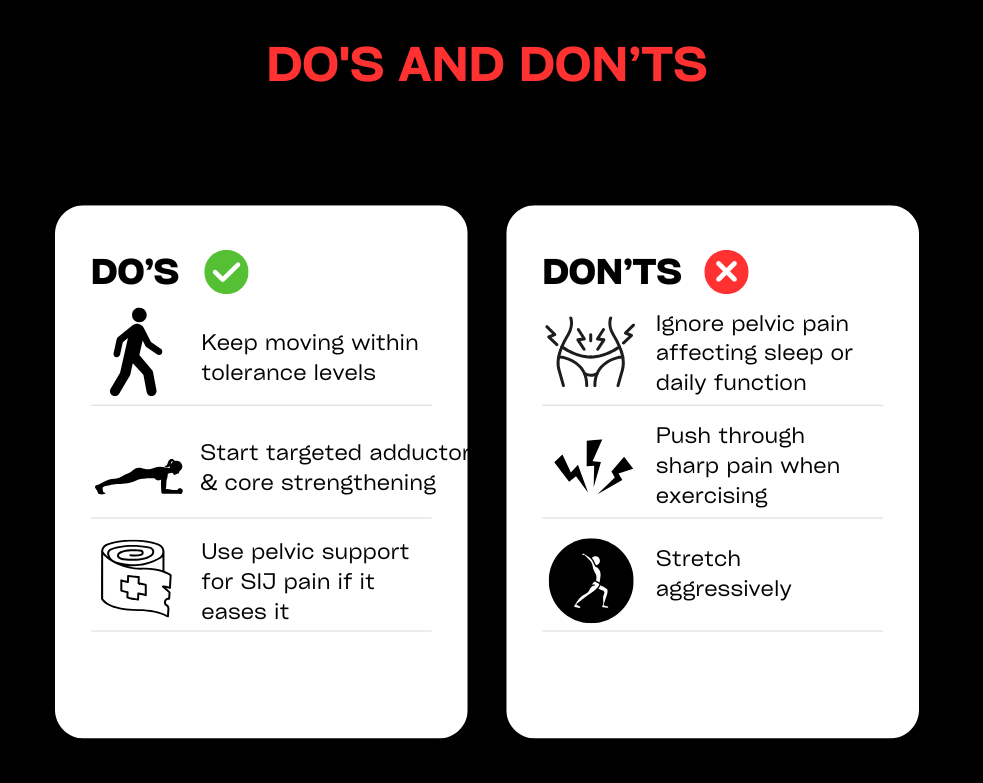
6. SELF-HELP & PREVENTION
- In the early phase, reduce high-impact activities like sprinting and deep lunges, but stay active with comfortable movements like walking or cycling.
- Begin gentle range-of-motion and pain-free isometric exercises, such as adductor squeezes or core activation, before progressing to controlled strengthening.
- Always warm up thoroughly, including adductor-specific drills, before sports involving kicking or changing direction.
- For SIJ discomfort, you can try a pelvic support belt, practise “log-rolling” to get in and out of bed, and avoid prolonged standing on one leg in the early stages.
- Focus on building well-rounded hip and core strength, address any asymmetries, and prioritise sleep and recovery.
7. WHEN TO SEE A PHYSIO OR SPECIALIST
- If pain continues for more than 2–4 weeks or keeps coming back when you return to sport.
- If you have sharp groin pain accompanied by a palpable lump or bulge, or associated testicular pain, which requires a medical review to rule out a hernia.
- If you experience red flag symptoms such as night pain, fever, unexplained weight loss, or neurological changes.
- If you experience marked instability or are unable to put weight on your leg after an injury.
- For any postpartum pain that interferes with your daily function or ability to care for your baby.
Hamstring injuries
1. DEFINITION & ANATOMY
A hamstring injury is a strain or tear affecting the group of three muscles at the back of the thigh (biceps femoris, semitendinosus, and semimembranosus). These injuries typically occur via one of two common mechanisms: high-speed running, where the muscle is rapidly overloaded as the leg swings forward, or a stretch-type injury from movements like kicking, high-stepping, or doing the splits. In some cases, the injury can involve the proximal hamstring tendon, which attaches the muscles high up on the “sit bone” (ischial tuberosity). A correct diagnosis of the grade and mechanism of injury is essential for guiding an effective rehabilitation plan.
2. SYMPTOMS & SIGNS
- A sudden, sharp pain felt in the back of the thigh.
- A distinct pulling or tearing sensation at the time of injury.
- Difficulty running, accelerating, or even walking normally.
- Tenderness when pressing along the length of the muscle or tendon.
- Bruising and/or swelling appearing on the back of the thigh, sometimes tracking down towards the knee.
- Stiffness and discomfort after periods of rest.
- Pain when performing a straight-leg raise or attempting to stretch the hamstring.
- Pain when resisting knee bending (flexion) or pushing the leg backwards (hip extension).
- Reduced sprint speed or a feeling of lost power.
- For proximal injuries near the sit bone, symptoms can include a deep buttock pain and significant discomfort when sitting.
3. CAUSES & RISK FACTORS
- Having a previous hamstring injury is the single biggest risk factor.
- An inadequate warm-up before intense activity.
- Rapid increases in training volume or speed work.
- Poor hamstring strength, especially eccentric strength (the muscle’s ability to lengthen under control).
- A strength imbalance where the quadriceps are much stronger than the hamstrings.
- Reduced hamstring flexibility or limited hip mobility.
- Weakness in the supporting gluteal and core muscles.
- Poor running or sprinting mechanics.
- General fatigue or inadequate recovery between training sessions.
4. HOW PHYSIOTHERAPY HELPS
- Assessment: We perform a thorough evaluation to grade the strain (I-III), identify the mechanism (sprint vs. stretch), and locate the exact site of injury. We also screen for more significant issues like proximal tendon involvement or a potential avulsion injury.
- Acute Care: We guide you on a plan of relative rest and pain-modulated loading, using compression to manage swelling. We advise on crutch use if needed and educate you on why aggressive stretching should be avoided in the early stages.
- Progressive Loading: Your recovery will be built around a phased exercise programme. This starts with gentle isometrics and progresses to eccentric strengthening (like Nordic curls and Romanian deadlifts) and lumbopelvic control exercises, building a robust foundation for your return to activity.
- Running Rehabilitation: We provide a structured, criteria-based return-to-running plan. This involves specific drills, building up stride length and speed, and safely reintroducing acceleration, deceleration, and changes of direction.
- Mobility & Adjuncts: We use gentle neural and soft-tissue techniques to restore pain-free movement without provoking symptoms. Manual therapy and taping may be used as needed to support your recovery.
- Education: A key part of our role is to teach you about load management, effective warm-up strategies, and how to recognise muscle soreness vs. pain, empowering you to prevent a recurrence.
5. TIMELINE / EXPECTED RECOVERY
- Grade I (Mild): Daily function often returns within 1–3 weeks. A return to running and sport typically takes 2–4 weeks or more with consistent rehab adherence.
- Grade II (Moderate): Recovery usually takes 4–8 weeks, though this can be longer depending on the demands of your sport and the specific injury location (stretch-type injuries can be slower).
- Grade III (Severe) / Suspected Avulsion: These injuries require 8–12 weeks or more. Some cases may need medical imaging and a specialist review.
- Following an early, criteria-based rehabilitation programme is the most effective way to reduce the high risk of re-injury.
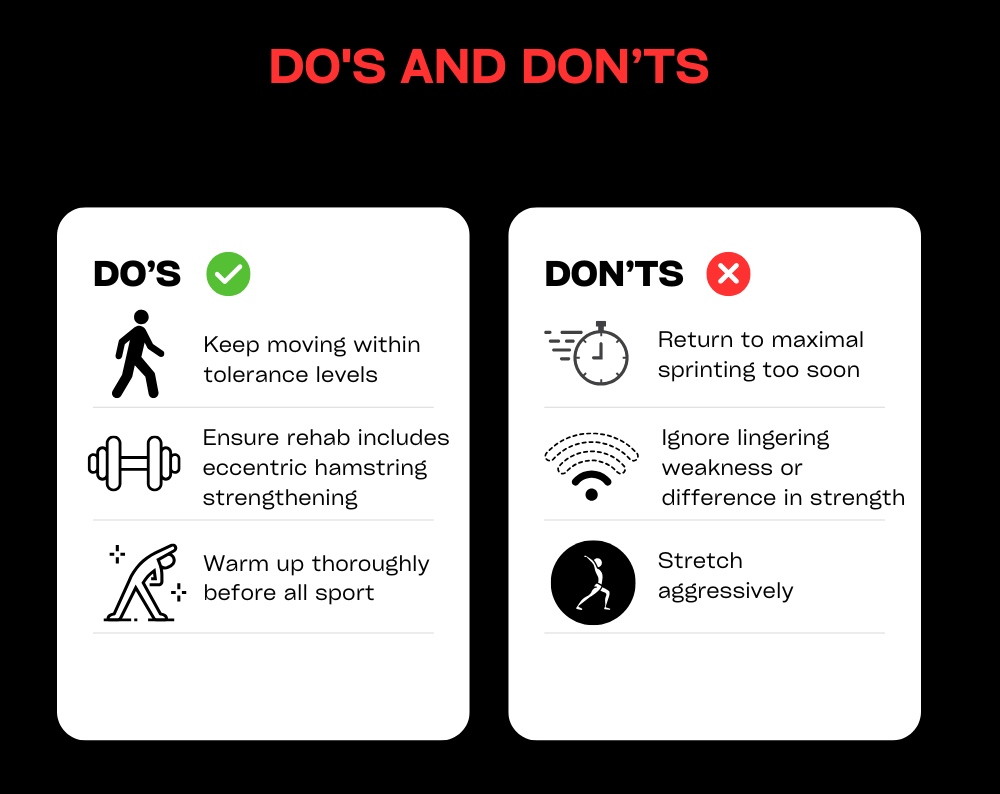
6. SELF-HELP & PREVENTION
- In the first 48–72 hours, focus on protection, relative rest, and compression. Avoid aggressive stretching, especially if the injury occurred during a stretch.
- Begin gentle, pain-free isometric contractions as advised. Progress to eccentric strengthening exercises (like Nordics, sliders, and RDLs) alongside your glute and core work.
- Reintroduce running gradually, following a walk-jog plan before moving to strides and faster speeds. Avoid maximal sprinting until the final stages of your rehabilitation.
- Always warm up thoroughly before sport, including hamstring-specific preparation drills, and maintain good hip mobility.
- Pay attention to your overall training loads, recovery, and sleep to prevent fatigue-related injuries.
7. WHEN TO SEE A PHYSIO OR SPECIALIST
- If you experienced a “pop,” have severe pain, significant bruising or swelling, or are having difficulty walking.
- If your pain is located very high up near the sit bone or if sitting is extremely uncomfortable, as this may indicate proximal tendon involvement.
- If pain persists beyond 2–3 weeks, you suffer from recurrent strains, or you are uncertain about the severity of the injury.
- If you have a sudden loss of strength, can see a visible defect in the muscle, or cannot bend your knee or push your leg back against resistance.
Headache
1. DEFINITION & ANATOMY
Headaches have many different causes and subtypes, including tension-type, migraine, cluster, and cervicogenic (neck-related) headaches. Physiotherapy is most effective for treating tension-type and cervicogenic headaches, and can also play a key role in managing the frequency and severity of migraines alongside medical care. Many headaches are influenced by the anatomy of the neck and shoulders. The joints of the cervical spine, key muscles like the upper trapezius and suboccipitals, and the jaw (temporomandibular joint or TMJ) can all refer pain into the head. A careful assessment is vital to classify your headache type, screen for any red flags, and tailor a treatment plan that addresses the true source of your symptoms.
2. SYMPTOMS & SIGNS
- Tension-Type: Usually a bilateral (both sides) pressure or a feeling of a tight band around the head. The pain is typically mild-to-moderate and is not worsened by routine activity.
- Cervicogenic: Often a one-sided pain that starts in the neck or at the base of the skull and spreads to the front of the head. It is commonly associated with reduced neck movement and tenderness in the upper neck muscles.
- Migraine: Typically a throbbing or pulsating pain, often on one side of the head, which is aggravated by activity. It is frequently accompanied by nausea, and sensitivity to light (photophobia) or sound (phonophobia).
- Cluster: A severe, one-sided pain usually felt around the eye or temple, accompanied by autonomic signs like a watery eye or nasal congestion on the same side. This type requires urgent GP or neurology input.
- TMJ-Related: A headache felt in the temples, often associated with jaw pain, clicking, or morning tightness in the jaw muscles.
- General Features: Many headache types can be associated with neck and shoulder stiffness, muscular trigger points, disturbed sleep, and can be linked to stress.
3. CAUSES & RISK FACTORS
- Prolonged desk work with poor ergonomics or sustained postures.
- Neck strain from an old injury, such as whiplash.
- High levels of stress or anxiety.
- Poor sleep quality or disruption to your sleep routine.
- Bruxism (unconscious teeth grinding or jaw clenching).
- Dehydration or missing meals.
- Hormonal factors, which can be a significant trigger for migraines.
- Overuse of pain medication.
- Lack of regular physical activity.
- Incorrect prescription for eyewear or other vision issues.
4. HOW PHYSIOTHERAPY HELPS
- Assessment: We perform a thorough examination to classify your headache type and screen for any red flags. This includes a review of your posture and workstation, a detailed cervical spine and TMJ exam, and guidance on using a headache diary.
- Manual Therapy: We use hands-on techniques such as joint mobilisations for the neck and upper back, soft-tissue release for tight muscles, and specific techniques for the suboccipital and TMJ areas to relieve tension and restore movement.
- Exercise Therapy: We prescribe a tailored programme of neck and shoulder blade strengthening exercises, deep neck flexor training, and mobility drills. We also incorporate breathing and relaxation strategies.
- Education: A key part of our approach is empowering you with knowledge. We provide advice on managing triggers, setting up your workstation correctly, and simple self-release techniques you can use at home.
- Adjuncts: Where appropriate, we may use taping for postural support, advise on heat or ice application, and liaise with your GP regarding medication or specialist referral.
5. TIMELINE / EXPECTED RECOVERY
- Tension-Type/Cervicogenic: With consistent adherence to exercises and ergonomic changes, many people experience significant improvement within 4–6 weeks.
- Migraine: As part of a multidisciplinary plan, physiotherapy can help reduce the frequency and severity of migraines over a period of 6–12 weeks or more.
- Chronic Cases: Long-standing or complex headache conditions may require ongoing management. Regular physiotherapy “tune-ups” can be effective for maintaining improvements and preventing flare-ups.
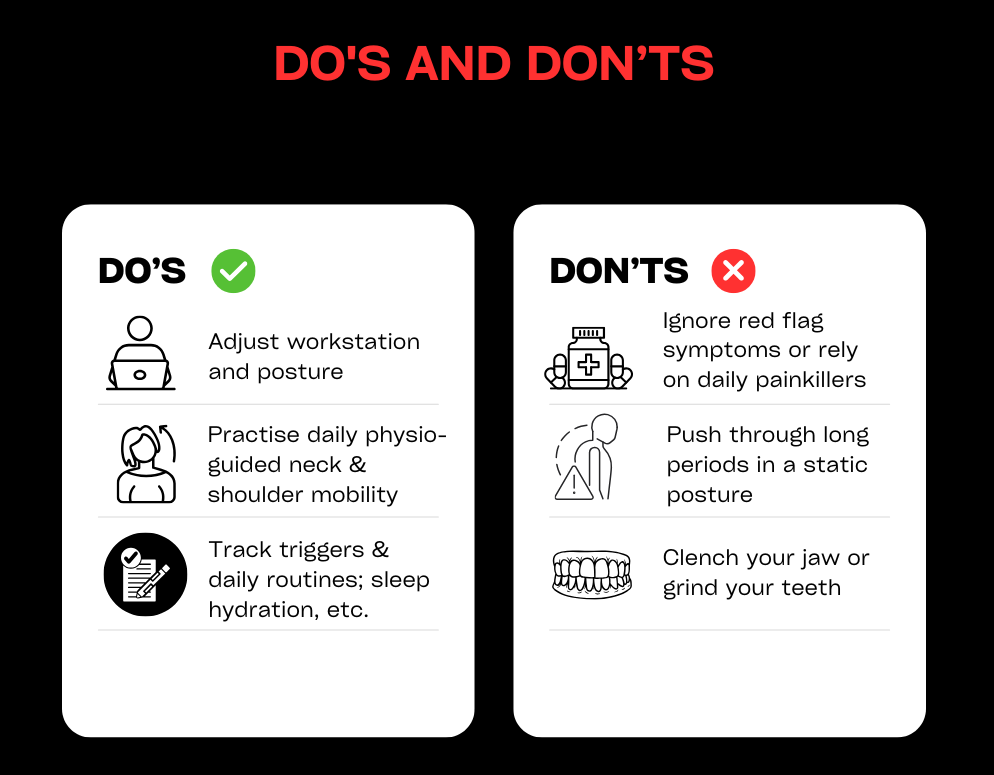
6. SELF-HELP & PREVENTION
- Keep a simple headache diary to track your symptoms and identify potential triggers related to food, activity, or stress.
- For desk work, follow the 20-8-2 rule: for every 20 minutes of sitting, try to spend 8 minutes standing and 2 minutes moving and stretching.
- Incorporate daily mobility and strength exercises like chin tucks, shoulder blade squeezes, and gentle thoracic extensions over a towel or foam roller.
- Optimise your lifestyle factors: ensure you are well-hydrated, eat regular meals, and get consistent, quality sleep.
- Actively manage stress with techniques like paced breathing, brief mindfulness exercises, or simply taking short breaks during a busy day.
- Review your workstation ergonomics and ensure your eyewear prescription is up to date. Consider using a headset for long phone calls to avoid neck strain.
7. WHEN TO SEE A PHYSIO OR SPECIALIST
- If you are experiencing new or changing headaches, or if your symptoms persist for more than 2–4 weeks despite self-care.
- Seek urgent medical review for any red flags: a sudden, “worst-ever” headache; new neurological symptoms (weakness, slurred speech, vision loss); fever with neck stiffness; a headache following a head injury; or a headache that comes on with exertion.
- If you have frequent migraines that are not well-controlled, it is important to see your GP or a neurologist. Physiotherapy can provide excellent support alongside medical therapy.
Jaw Pain / Clicking
1. DEFINITION & ANATOMY
Jaw pain and clicking are common symptoms of Temporomandibular Disorders (TMD), which affect the temporomandibular joint (TMJ), its disc, and the surrounding muscles. The TMJ is the complex hinge connecting your jaw to your skull, and it works alongside muscles like the masseter, temporalis, and pterygoids to allow you to talk and chew. Symptoms can include pain, clicking or popping sounds, limited opening, or locking. This can be caused by parafunction (like clenching and grinding), excessive gum chewing, poor posture, neck issues, trauma, or stress. Physiotherapy can be highly effective by addressing joint mobility, muscle tension, and the daily habits that contribute to the problem.
2. SYMPTOMS & SIGNS
- Pain in the jaw, temples, or in front of the ear, especially with chewing, yawning, or talking.
- Clicking, popping, or grinding sounds when opening or closing your mouth.
- Episodes of the jaw locking open or closed, or a limited ability to open wide.
- Morning stiffness or soreness in the jaw muscles, often linked to night-time grinding (bruxism).
- Tenderness when pressing on the main chewing muscles on your cheek (masseter) or temple (temporalis).
- Headaches, particularly in the temples.
- Earache, ringing, or a feeling of fullness in the ear without any sign of infection.
- Associated neck and shoulder tension or pain.
- The jaw deviating to one side when you open your mouth.
3. CAUSES & RISK FACTORS
- Teeth grinding or clenching (bruxism), which is often linked to stress and anxiety.
- Habits like prolonged gum chewing, eating very hard or chewy foods, nail-biting, or pen chewing.
- Poor posture, especially a forward head position during prolonged screen time.
- Recent extensive dental work or changes to your bite.
- A direct trauma or blow to the jaw or face.
- Underlying neck dysfunction that refers pain to the jaw.
- Disrupted sleep patterns.
- Generalised joint hypermobility.
4. HOW PHYSIOTHERAPY HELPS
- Assessment: We conduct a thorough assessment to screen for any red flags, examine your jaw’s movement pattern, and check for joint noise or pain. We also assess your neck posture and habits, and will liaise with your dentist or GP if needed.
- Manual Therapy: We use hands-on techniques including TMJ mobilisation and targeted soft-tissue release for the chewing muscles (masseter, temporalis, pterygoids). We also treat the neck and suboccipital muscles to reduce referred pain.
- Exercise Therapy: We will prescribe a specific programme of exercises, including controlled jaw opening and closing drills, gentle isometrics, and postural strengthening for your neck and shoulder blades.
- Education & Habit Change: A crucial part of recovery is learning to manage the condition. We provide strategies for bruxism, relaxation, sleep hygiene, and diet modifications (like eating softer foods initially). We also offer ergonomic advice for your workstation and phone use.
- Adjuncts: We can use taping to provide postural cues and will coordinate with your dentist if a night guard for bruxism is recommended.
5. TIMELINE / EXPECTED RECOVERY
- Many people with mild-to-moderate TMD feel a significant improvement within 4–6 weeks of starting physiotherapy, provided they are consistent with their exercises and habit changes.
- Long-standing or more complex cases may take 8–12 weeks or longer to resolve. These cases often benefit from combined care with a dentist or a psychologist for stress management.
- Flare-ups are common with TMD, but once you have effective self-management strategies in place, they usually settle much faster.
6. SELF-HELP & PREVENTION
- During a flare-up, avoid extreme jaw opening, tough or chewy foods, and chewing gum. Cut food into smaller pieces to reduce strain.
- Practise a relaxed jaw posture throughout the day: keep your lips together, teeth slightly apart, and let your tongue rest gently on the roof of your mouth.
- Apply a warm pack to your jaw, temples, or neck for 10–15 minutes. You can also perform gentle self-massage to the main cheek (masseter) and temple muscles.
- Take regular posture breaks from your desk and practise chin tucks and shoulder blade squeezes. Limit cradling your phone between your ear and shoulder.
- Actively manage stress, especially before bed. Try paced breathing exercises and aim for a consistent sleep routine.
- If you suspect you grind your teeth at night, discuss getting a custom bite guard with your dentist.
7. WHEN TO SEE A PHYSIO OR SPECIALIST
- If your jaw pain, clicking, or locking persists for more than 2–4 weeks despite self-care.
- If your jaw locks open or closed, you have recurrent dislocations, or your opening is severely limited (less than about three fingers’ width).
- Seek urgent medical review for any red flags like a suspected fracture or infection, fevers, sudden unexplained swelling, or neurological symptoms.
- If you have severe tooth pain or sudden changes to your bite, see a dentist first. Combined care between a physio and dentist often yields the best results.

Knee Pain/Patellofemoral pain (PFJ)
1. Definition & Anatomy
Patellofemoral pain (PFJ pain) refers to discomfort around or beneath the kneecap (patella). It often occurs due to how the patella moves (or “tracks”) within the femoral groove during activities like walking, running, or squatting. The condition can involve irritation of the cartilage under the kneecap, leading to pain and inflammation.
2. Symptoms & Signs
- Pain when squatting, climbing stairs, or sitting for long periods (commonly called the “theatre sign”).
- Clicking or grinding sensations under the kneecap.
- Swelling, aching, or stiffness in the knee.
3. Causes & Risk Factors
- Overuse or repetitive stress: Activities like running or jumping can overload the knee.
- Poor hip/core strength: Weakness in these areas can lead to poor knee alignment.
- Flat or overpronated feet: This can alter biomechanics and increase strain on the knee.
- Muscle imbalances: An imbalance between the vastus medialis and lateralis muscles can affect patella tracking.
- Sudden increases in activity: Rapidly increasing running distance or intensity can trigger symptoms.
4. How Physiotherapy Helps
- Assessment: A physiotherapist will evaluate your gait, hip and foot biomechanics, strength, and flexibility.
- Treatment Plan: This may include manual therapy, taping, and exercise therapy to improve strength and stability.
- Load Management: Temporary modifications to activities to reduce strain on the knee.
- Modalities: Techniques like ultrasound or other clinic-specific treatments may be used to reduce pain and inflammation.
5. Timeline / Expected Recovery
- Mild cases: With consistent physiotherapy and adherence to exercises, improvement is often seen within 4-6 weeks.
- Severe or long-standing cases: Recovery may take several months, especially if cartilage damage is involved.
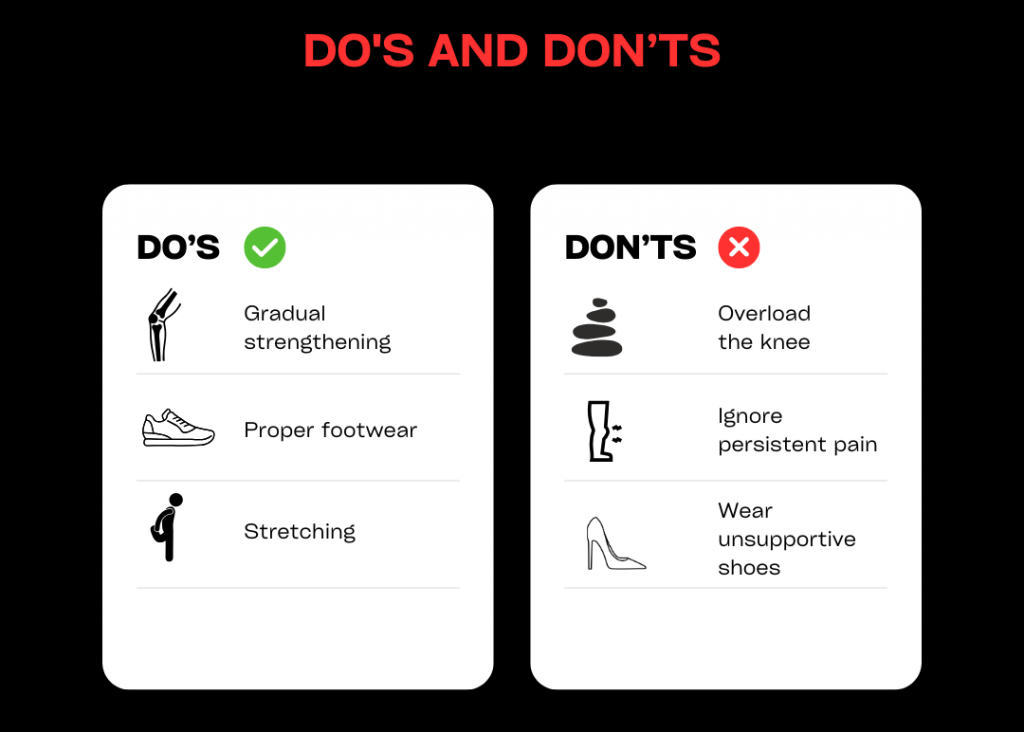
6. Self-Help & Prevention
- Strengthen key muscles: Focus on hips, quads, and glutes.
- Stretch tight areas: Pay attention to the IT band, hamstrings, and calves.
- Wear proper footwear: Consider orthotics if needed.
- Avoid rapid increases in activity: Gradually build up running or stair-climbing.
- Use ice and rest during flare-ups to manage pain.
7. When to See a Physio or Specialist
- If pain persists for more than 4-6 weeks without improvement.
- If you experience severe pain, locking, or the knee giving way.
- If you suspect ligament or meniscus involvement.
Don’t let knee pain hold you back. If you’ve been experiencing symptoms for more than 3-6 weeks or your pain is getting worse, book an appointment with one of our physiotherapists today. Let us help you get back to doing what you love, pain-free.
Lower back pain / piriformis syndrome
In the UK, up to 80% of people will experience back pain during their lifetime (NICE.org.uk). This equates to almost £5bn per annum through missed days of work, reduced hours or decreased productivity (britishpainsociety.org). Back pain can be split into several sub-categories – from disc related pain, mechanical (or muscle and joint) pain, neurogenic (nerve) pain, and metastatic (cancer) pain. At W5Physio, we’ll quickly diagnose your back pain before tailoring treatment to your specific needs.
You don’t need to live with lower back pain. Get in touch with us today.
Metatarsal injuries
Metatarsal (MTP) injuries can be the result of direct trauma (e.g. a stamp on the foot) or overload due to poor foot biomechanics or weak muscles in the foot and lower leg. It’s also important to exclude stress fractures before we start treatment, so we’ll carry out a full consultation to find the precise cause of your injured metatarsal.
Book your slot today to find out more.
Mid back pain (thoracic)
Stiffness, aching or sometimes sharp pain can all be experienced in the mid to upper back. Overusing the muscles or ligaments in this area can be to blame as can sitting in the same position for a prolonged period of time (e.g. at a desk or when driving a car).
Pinched nerves or osteoarthritis can further be to blame, and less common are things like herniated discs or fractured vertebrae.
We treat a lot of patients with mid back pain with great success. Don’t suffer in silence… come and get some professional advice and relief from one of our experienced physios.
Neck pain
Neck pain will affect two thirds of the UK population over their lifetime, with 75% of sufferers having a relapse within five years (Arthritis Research UK). Common causes of neck pain include non-specific neck pain (mechanical pain), whiplash, spondylosis (arthritic neck pain) and acute torticollis (sudden seizing of the neck, often in the morning after a poor or cold sleep). As with lower back pain, we’ll diagnose the exact cause of your pain and symptoms, before treating you pain accordingly.
Get moving and reduce pain quickly. Book an appointment with one of our physios.
Posterior ankle pain / heel pain / fat pad
Posterior ankle pain can be the result of a small sack of fluid called the retrocalcaneal bursa, problems with the Achilles tendon or a condition called tibialis posterior tendonitis. Occasionally, traumas such as twisting the ankle or a poor football tackle can fracture to the talus bone, and a small piece of the bone is left in the ankle joint. It’s important to exclude this before starting any treatment, so don’t put off a professional diagnosis with any ankle strain or sprain.
Book an appointment today for expert advice on ankle pain.
Posterior knee pain
Posterior knee pain can be due to local structures i.e. the popliteal muscle, bursae as well as muscles that attach at the back of the knee (hamstring and calf muscles). It is important to check the menisci and ligaments as these can refer pain to the back of the knee. We’ll examine you before providing an accurate diagnosis.
Knee pain is one of the most common complaints we help in clinic. Book to see us today.
Shin splints
Shin Splints, also referred to as medial tibial stress syndrome (MTSS). occurs with overload to the muscles in the area. As you can imagine, the muscles in the lower leg are designed to work hard and don’t injure easily. But MTSS was first recognised in Army recruits going from a little, to a lot of activity and this is common factor we’ll to look out for when diagnosing MTSS. Pain on the inside of the shin, sometimes with lumps on the bone that are painful to touch are further symptoms.
It’s a slightly rarer complaint, but physiotherapy can definitely help. If you suspect shin splints, make an appointment with us.
Shoulder pain – impingement / instability
The shoulder is a complex joint that allows lots of movement to the expense of stability. Therefore, there are two main problems: impingement – things getting pinched in the joint; and instability – where the top of the arm bone (humerus) rattles around too much. It’s common to see the two side-by-side other.
Other shoulder issues include labral tears, bursitis, plus a whole host of other complicated causes. Finding the underlying cause of shoulder problems can be difficult, but our experienced team is here to help.
Make an appointment to see us today with your shoulder pain.
Tennis elbow / Golfers’ elbow
Tennis elbow is on the outside, Golfers’ elbow on the inside. They’re both tendon problems related to corresponding muscles. When you visit W5Physio, we’ll look at both internal (i.e. forearm extensors) and external factors (i.e. your technique) to identify the exact cause and source of your pain.
We’ll help you find a solution that’ll alleviate your pain and prevent the problem returning. Book an appointment today.
Thigh strains and ITB syndrome
Thigh strains and Iliotibial Band Syndrome (ITB) can present themselves as a slight strain to the muscle fibre (Grade I), through to a complete rupture (Grade III). A complete rupture can sometimes take between nine and 12 months to heal, so don’t put off an appointment for thigh strains and ITB issues.
Book to come and see us ASAP.
Whiplash
Whiplash is a nasty injury that can result in different types of pain (nerve pain or neurogenic, inflammatory pain, mechanical or mechanical nociceptive pain). Different structures i.e. the joints, muscles or nerves react to whiplash in differing periods of time and patients can sometimes be surprised that whiplash symptoms don’t always appear at once. The sooner you get whiplash looked at the more likely you are to prevent any long-term problems.
Book an appointment with one of our physios today.
Women’s pelvic health/Mummy MOT
Almost half of all women experience weakness in both the pelvic floor and abdominal muscles post pregnancy. Pelvic health issues are also common during perimenopause and menopause. Left untreated, these problems persist and can lead to pelvic pain, back pain and bladder/bowel or sexual dysfunction. These conditions should not be something you just put up with because of having a baby or going through the menopause. So much can be achieved through the correct knowledge, treatment and exercise.
Learn more about the Mummy MOT here. Or, book in today for the health check you deserve.
Wrist pain / strain
We see a lot of wrist pain and strains in our practice. From people who have fallen and experienced trauma to the wrist as they’ve put their hand out to stop themselves, to sports players who have injured themselves on the tennis court, playing basketball or doing gymnastics.
Of course, wrist pain related to repetitive movements is also really common as most of us spend lots of time on mobile phones, typing on keyboards or holding a computer mouse.
The good news is physio has great success rates for wrist problems. So don’t delay in booking to see us with your wrist pain/strain.
Your First Visit
Diagnose
On your first visit we’ll ask you lots of questions to identify the best course of action and make sure physio can help you.
We’ll need access to the body part causing issues, so remember to wear suitable clothing so that we can carry out some physical tests.
Treat
In your first session, we’ll normally start treatment too. It’ll be tailored to you specific needs and condition.
It could include hands-on manipulation, prescribed exercises and sometimes also sports massage or acupuncture.
Cure
Curing you means working with you, rather than simply telling you what to do. We aim to achieve long-lasting results with every single patient, so expect a personal, bespoke treatment plan and approach.
Meet Our Team
Client Reviews
Toni
The service and care that the W5 team offer their clients is absolutely first class. Professional...
GIAMPIERO
Excellent experience, and even better result, thanks to great competence, equipment and availability. Highly recommended. Big...
Madolyn
Personal service, amazing advice and the whole support team are a dream. Thank you!
Al
I've been a patient of Stewart R & Greg B for too many years to remember....
In Partnership With